
Mohamed A. Elhawary
Vaccine Safety Officer, Lecturer, and General Secretary of the ISoP Egypt Chapter, Ministry of Health & Population

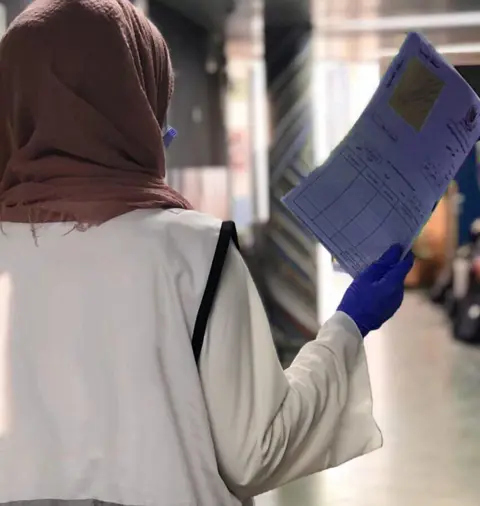
Photo: iStock
A universal problem for refugees is the loss of vital health records. ISoP Egypt Chapter and the Palestine Red Crescent Society are taking on this problem to reduce medication errors and improve reporting practices.
When it comes to providing complete patient medical information at the point of medical care, we continue to find a significant number of referrals associated with preventable medication errors. In particular, we see this among Palestinian refugees, who fled or were driven from their homes in the Gaza Strip to Egypt, seeking medical assistance or primary health-care facilities. Much of this support for the registered Palestine refugee population in Egypt is provided through the Palestine Red Crescent Society (PRCS) whose Egypt branch operates Palestine Hospital in Cairo (PHC). But for these patients, the paper-based referral system makes it quite difficult for primary care providers (PVPs) to follow-up on referral letters to specialists, ensure better care coordination between providers, and improve the overall effectiveness of the referral tracking process.
One of the hindrances to instant communication of patient information is the confusion provoked by perpetual and severe shortages in medications. These shortages jeopardise the life of patients in the Gaza Strip and, accordingly, may give rise to medication errors, adverse drug reactions (ADRs), and other complications. Though there is plenty to list, the potential risks that medication shortages pose to patient safety include non-optimal or analogue substitute of the same medicine entity being dispensed (such as telmisartan/hydrochlorothiazide instead of telmisartan in older hypertensive patients with a secondary diagnosis of dehydration). Furthermore, PHC’s healthcare workers who are unable to access an easy-to-find, clear, and comprehensive patient medical information can face confusion about or misunderstanding of the distinct difference between adverse patient outcomes of analogue alternatives and adverse reactions related to comorbid conditions.
“The paper-based referral system makes it quite difficult ... to follow-up on referral letters to specialists, ensure better care coordination between providers, and improve the overall effectiveness of the referral tracking process”
The current conditions also mean that medication errors are more likely to occur at all stages – from injecting the medication into the wrong route or administering excessive doses of an agent, through to prescribing an incorrect drug that is less effective, has a worse adverse-effect profile, or involves a complex dosing schedule. Movement restrictions on medical supplies to the Gaza Strip have also exacerbated pre-existing conditions, such as inaccurate substitutions of whole medication regimens and administration of out-of-date or expired medicine that jeopardises patient safety. Power outages in Gaza also continue to disrupt essential health services for at least two million Palestinians, including the stability of vaccines and other pharmaceuticals.
With medication errors and adherence challenges faced by patients from refugee backgrounds gaining greater recognition as an integral component of patient safety culture, the Egypt Chapter of the International Society of Pharmacovigilance (ISoP) organised a medication errors training course targeting hospital pharmacists. The designated workshop, held in January 2021, aimed to raise attention to the problem of medication errors and highlight the potential contributing factors. In addition, it focused on equipping healthcare providers (HCPs) with the knowledge and skills to conduct an operational assessment, evaluate potential impact on patient care, and ultimately use their investigation to develop a risk reduction strategy.
After attending the ISoP Egypt Chapter medication errors training course, the pharmacy department in the PHC, decided to put the lessons they had learned into practice. This led to an effective initiative to effectively tackle potential medication-related errors by creating an executable framework and a well-defined therapeutic management strategy. The action plan adopted by the PRCS to improve patient safety, aims to facilitate improvements in ordering, receiving, dispensing, and supplying medicines. It also addresses the challenges of providing humanitarian aid to thousands of patients living with disabilities.
In the context of accurate medication use and decreased errors, the Egyptian Chapter of ISoP engaged in developing a streamlined electronic health record (EHR) software that renders patient medical information (including medical history, previous surgeries, treatment plans, and other data) available instantly to PHC’s healthcare workers and PRCS branches in Jordan, Lebanon, and Syria. As such, the management of patient clinical data derived largely from internal event reporting and conceived to substantially improve a hospital’s medication safety would result in better care coordination of strategies in both the inpatient and outpatient settings.

All in all, administrative staff in charge of entering patient data into the medical records were trained on how to manage databases to store and retrieve data, whereas selected members of clinical staff were instructed how to interpret information about an aspect of patient care and to look at the prevalence and effectiveness of their designated treatment. The application of a robust computerised medication errors reporting system has been deemed successful as a means of capturing and disseminating information on safety events rapidly and in real time. PHC’s HCPs along with administrative staff should continue to preserve their capacity for effective adaptation in terms of coping with changing technology trends and investigating new approaches to drug safety.
The authors acknowledge the kind support of DigiMed Technologies for remodelling new amendments to PHC’s management system. The authors also wish to thank all international experts who collaborated in the design and delivery of our training course under the umbrella of ISoP Egypt Chapter.
The annual #MedSafetyWeek campaign reminds us that medicines work best when they're safe. In Aligarh, healthcare workers came together to make that message a living reality.
19 November 2025
Since 2020, the ICPV has worked to improve drug safety reporting at Instituto Nacional de Cardiología Ignacio Chávez, with promising outcomes.
16 October 2025
Two-thirds of pharmacists in Nigeria witness weekly cough syrup abuse, yet poor reporting systems and unclear guidelines prevent effective intervention, leaving its youth at risk.
03 December 2025