
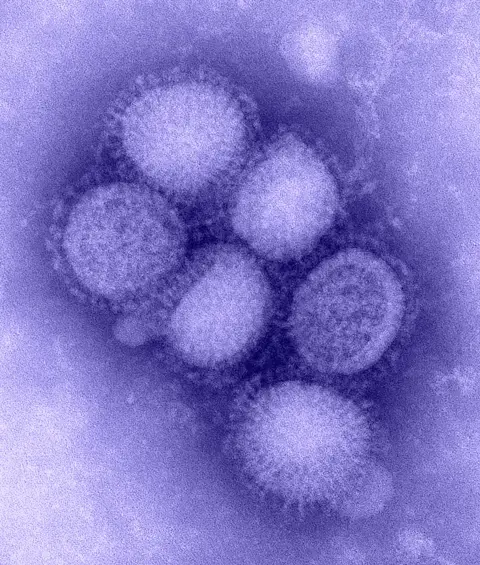
It’s been said that history does not repeat itself, but it does often rhyme. In the case of the COVID-19 pandemic, it appears, the rhyme can also amplify the past. For Uppsala Monitoring Centre’s recently retired chief medical officer, Pia Caduff-Janosa, the rhyme she hears most clearly is with the 2009 H1N1 pandemic, the swine flu outbreak that spread around the world from early 2009 to mid 2010.
Although the 2009 event proved far less deadly or disruptive than our current crisis, the experience of a decade ago provided valuable lessons. In particular, several of the pharmacovigilance approaches and systems developed then could prove vital now as the global health community prepares for what may well become the most intensive and large-scale vaccination programme ever conducted.

As Caduff-Janosa was wrapping up her 8-year tenure at UMC, she sat down with Uppsala Reports to discuss how her previous role helped pave the road down which UMC now travels as it seeks to provide critical pandemic-related safety surveillance for both treatments and – as now seems likely – new vaccines.
In 2009, Caduff-Janosa was 10 years into a 13-year career at the Swiss Agency for Therapeutic Products (Swissmedic), the Swiss national surveillance authority for medicines and medical devices. At that point, she was head of the Vigilance Unit in the Division of Drug Safety, responsible for post-marketing surveillance of medicines for human and animal use as well as haemovigilance.
Caduff-Janosa described her agency as well-funded and highly respected, with strong support from national institutions and external stakeholders – factors that would prove critical in its efforts to lead the way in real-time vaccine monitoring. One of the stakeholders that Swissmedic worked closely with was UMC, and a major part of their collaboration involved VigiFlow, UMC’s web-based management system for recording, processing, and sharing reports of adverse effects.
“H1N1 is an influenza-type virus, so we expected the wave of infections to hit during the normal flu season,” Caduff-Janosa said.
“That meant we had some time to react and prepare for real-time monitoring of any vaccine that was approved.”
“We had some time to react and prepare for real-time monitoring of any vaccine that was approved.”
Indeed, there were multiple vaccines being developed for H1N1. But an early concern, based on the experience of H1N5 avian flu vaccine development, was that the H1N1 vaccines may need to be administered in multiple doses, weeks apart, for optimal efficacy. Developing a new vaccine is one challenge. Scaling up production of such a vaccine to cope with the demand of a pandemic is at least as daunting. And if multiple doses are required to protect individuals, then the challenges of both supply and dose compliance can threaten to undermine the chances of success.
So, to improve efficacy and, therefore, reduce the production demand, some variants of the vaccines used an adjuvant – a substance designed to boost the immune system’s response to the antigen in the vaccine, enabling protection with a single dose. While adjuvants have existed in different forms for many decades, the proprietary squalene-based adjuvants being used in the H1N1 vaccines were relatively novel at the time.
“We knew there would be a need to vaccinate large numbers of people quickly,” Caduff-Janosa said.
“Because there would be entirely new products being used at great scale, it would be necessary to monitor in real-time and be able to report on any problems as quickly as possible.”
In this context, Swissmedic, which was already using VigiFlow, commissioned UMC to develop new tools. Swissmedic collaborated closely on the development, resulting in the emergence of the PaniFlow software.
“The idea of PaniFlow was not to get a complete set of data on vaccine-related events, but rather to secure a rapid flow of reports that could be followed up on if signals were detected,” Caduff-Janosa said.
“Every time there is a mass administration of a drug or vaccine, you have to be aware that you are giving it to people who may have contraindications and you can’t always make informed individual decisions. To intervene in a timely fashion, you need to monitor in real time,” she said.
In the words of a WHO Drug Information newsletter from 2009, PaniFlow enabled countries to “quickly detect potential safety problems in their own populations and take remedial action if causality is established. At UMC, the global picture can be rapidly reviewed and the international community alerted when problems are suspected or confirmed”.
Nowadays, with the approach and features of PaniFlow incorporated into VigiFlow and VigiBase, it’s clear that the experience of the 2009 pandemic has gone a long way to preparing the global pharmacovigilance community for the challenges present and emerging in COVID-19.
Caduff-Janosa suggests another approach that could be used to boost pandemic-related signal detection activities is to set up “beacons”. By concentrating pharmacovigilance resources in certain key locations, large amounts of data can be gathered, analysed, and extrapolated for broader investigation.
Despite the challenges that repurposed drugs and novel vaccines pose for patient safety, Caduff-Janosa is optimistic about the progress pharmacovigilance has made since the last pandemic. She points to the improvements in technologies and processes for signal detection and assessment and the increasingly sophisticated contributions that data scientists are making to the field. Reporting of adverse events has also improved.
“There were no mobile reporting apps 10 years ago,” she said. And the increased availability of training, including the delivery of short e-learning modules is another factor helping to improve the quality of both inputs and analysis, according to Caduff-Janosa.
“There’s so much more information now, and there is more and better research anchored in the reality of what’s required.”
But knowledge is worthless without dissemination. Effective communication, therefore, is a vital element of pharmacovigilance. In this respect too, Caduff-Janosa has observed considerable development over the past decade.
“Communication needs to be timely, accurate, truthful, and not kept in secret channels”
“The pandemic of 2009 helped us bring many different stakeholders onboard at the start of the process,” she said, noting that in the time since, international collaborations have continued to build and coordination among members of the WHO Programme for International Drug Monitoring has flourished.
“Communication needs to be timely, accurate, truthful, and not kept in secret channels,” she said, explaining that a positive example can be seen in the opening of VigiBase to the public via VigiAccess.
Caduff-Janosa’s career at UMC has been bookended by pandemic, and her contributions to both the organisation and the field of pharmacovigilance have been invaluable. Looking forward to the field’s future, she believes that the pharmacovigilance community has a greater role to play in vaccine safety than it has in the past. The coming months and years will be demanding, but she believes that the experts and institutions that make up the pharmacovigilance community will rise to the challenge.
As to her own future, Caduff-Janosa’s retirement brings a change of direction, as she prepares to start studying again, this time in the humanities, pursuing a degree in Eastern European and Jewish studies.




