
Maurício Perroud
Professor of Pneumology, School of Medical Sciences, Unicamp
Medical Director, Hospital Estadual Sumaré, Unicamp

At the Hospital Estadual Sumaré, extra safety measures help avoid medication errors, and an ME-prevention method based on the principles of signal detection is being investigated.
The Hospital Estadual Sumaré (HES) is one of the hospitals of the University of Campinas (Unicamp), a public university in the state of São Paulo, Brazil. The hospital was opened in September 2000, and it is an important centre for education and in-service training for students from the School of Medical Sciences.
HES was the first public hospital in Brazil to be certified with a higher grade in the Brazilian accreditation system for healthcare units, and the first hospital outside of the state capitals to be certified by the healthcare standards organisation Accreditation Canada, again at a higher level. Quality management is an important part of the hospital’s institutional culture. Following a recommendation by the regulatory authority of São Paulo, a pharmacovigilance commission was established in 2003 at the hospital, formed by a physician, a nurse, and a pharmacist. From the beginning, medication errors (MEs) were recognised as a specific issue that must be assessed separately from notifications related to suspected adverse drug reactions. Thus, several policies have been developed over the years, in order to reduce MEs at the hospital.
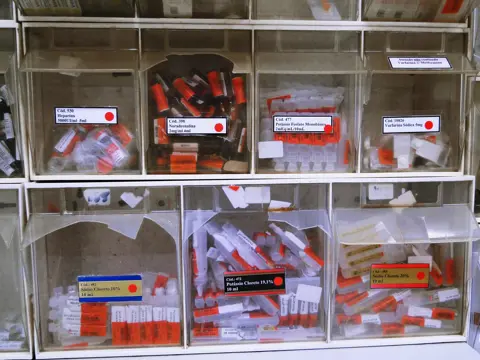
For each phase of the medicine-handling process – starting with purchase of products, through storage, prescription, drug dispensing from pharmacists, and finally drug administration – there are certain actions and safety measures that must be taken. For example, the qualification of suppliers is checked at the purchasing phase; ‘high alert’ drugs such as adrenaline and anesthetics are marked with a red label in the storage phase, and medicines are also sorted in a colour scheme by expiration date; the prescription phase calls for the use of standard prescriptions made according to medical protocols; and so on.
One action in particular should be highlighted: the prescription system for antimicrobial prophylaxis in surgery. There is a prescription protocol, but the physicians’ rate of compliance with it was low – less than 50% – until 2011. The problem was that they were asked to prescribe using the drug name, but as doctors usually work in two or more hospitals and each institution has its own protocol, inconsistencies occurred. At HES, a system was created where the physicians should prescribe the name of the medical procedure instead, for example cholecystectomy, which resulted in 100% compliance with the protocol.
“HES staff are studying whether the methodology used to conduct signal detection in pharmacovigilance could be used for ‘signal detection’ to prevent medication errors in hospitals.”
Two years ago, staff at HES discussed the introduction of a method to identify a risk and take early action to prevent MEs. This question is relevant because the assessment of the database is usually done by analysing the most frequent events. Focusing on this point, a pilot study was conducted, which became a research project.
In this project – which is still ongoing – HES staff are studying whether the methodology used to conduct signal detection in pharmacovigilance – namely the proportional reporting ratio methodology – could be used for ‘signal detection’ to prevent MEs in hospitals. To apply this methodology, all adverse events of one sector, e.g. the internal medicine ward, are compared with all adverse events of the other sectors. The pilot study was undertaken in 2015 on data collected between 2013–2014 and it was possible to identify a ‘signal’ for MEs. Now this methodology is promoted at HES using a database with more than 5,400 adverse events, excluding suspected adverse drug reactions, reported since January 2008. If the validity of this process can be proved, HES will start a prospective study.
Since 2020, the ICPV has worked to improve drug safety reporting at Instituto Nacional de Cardiología Ignacio Chávez, with promising outcomes.
16 October 2025
Two-thirds of pharmacists in Nigeria witness weekly cough syrup abuse, yet poor reporting systems and unclear guidelines prevent effective intervention, leaving its youth at risk.
03 December 2025
The annual #MedSafetyWeek campaign reminds us that medicines work best when they're safe. In Aligarh, healthcare workers came together to make that message a living reality.
19 November 2025