Deep dive
Preventing medication errors: a global challenge
Medication errors are a leading cause of avoidable harm in healthcare, affecting millions of people worldwide each year. These errors not only harm patients but also cost healthcare systems billions of dollars globally. By understanding the different types of errors and finding effective ways to prevent them, medication safety can be improved for everyone.

The scope of the problem
Medication errors harm 1 out of every 20 patients in healthcare.
The global cost of medication errors is around $42 billion annually.
50% of all avoidable harm in healthcare is caused by medications.
What is a medication error?
“A medication error is any preventable event that may cause or lead to inappropriate medication use or patient harm while the medication is in the control of the healthcare professional, patient, or consumer.”
– National Coordinating Council for Medication Error Reporting and Prevention

Critical stages for medication errors
Medication errors can happen at any point in the medication process, from prescribing to monitoring. WHO has found that at least 1 in 20 patients (5%) experience preventable medication-related harm globally. Understanding where errors occur can help guide the development of safeguards and procedures to prevent avoidable harm.
Prescribing
Errors occur when the wrong medication is prescribed, or when the correct medication is prescribed with the wrong dose, route, frequency, or duration.
Dispensing
Errors can happen during the preparation and dispensing of medications, such as providing the wrong medication or incorrect dosage.
Administering
Errors can occur when the medication is given to the patient, such as administering it at the wrong time or via the wrong route.
Storage
Medications can become less effective or unsafe if they are not stored correctly. This includes keeping them at the right temperature.
Monitoring
Patients risk being harmed if adverse effects are not detected, or necessary adjustments to the treatment are not made.
Those most at risk
Some people are more vulnerable to medication errors, particularly those who are elderly, children, or pregnant. By understanding and recognising the challenges these groups face, it’s possible to develop better ways to protect them.
Child patients
- Lack of paediatric guidelines: Many medications do not have specific dosing guidelines for children, making it difficult to determine the correct dose.
- Dispensing challenges: Medications prescribed for children often require precise calculations based on age, size, and weight, increasing the risk of dosing errors.
- Administration errors: Errors can happen when giving medicine, such as when a liquid dose isn’t measured accurately or when a child doesn’t receive the full amount.

Elderly patients
- Polypharmacy: Taking multiple medications increases the risk of drug interactions and side effects.
- Physical impairment: Elderly patients may have difficulties taking their medicines, such as swallowing tablets, opening packaging, or reading instructions.
- Adherence to complicated medication regimens: Complex medication schedules can lead to missed or double doses.
Pregnant patients
- Harm to the unborn baby: Some medications can cause birth defects or developmental issues in the foetus.
- Physical changes: Changes in the body during pregnancy can affect how medications are processed, leading to incorrect dosages.
- Mixing medications: Taking prenatal vitamins, supplements, and prescribed medications together can cause unexpected reactions.

Medication error reporting
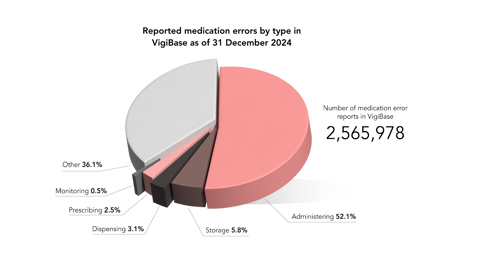
Medication errors happen at different stages of treatment. Between December 2019 and December 2024, the number of medication error reports in VigiBase, the WHO global database of adverse event reports for medicines and vaccines, more than doubled – from 1.2 million to 2.6 million.
Based on the most reported errors in VigiBase, these are the areas where errors most often occur, listed in order of frequency:
- Administering
- Storage
- Dispensing
- Prescribing
- Monitoring
Although reporting patterns vary across countries, these insights can help highlight key areas to focus on in your own healthcare setting.
Administration errors and the 5 rights of medication use
Global adverse event reporting patterns in VigiBase suggest that administration errors are the most common area of concern. The five rights of medication use – right patient, right drug, right time, right dose, and right route – are a good starting point for reducing administration errors, but more rights may be used in different settings based on specific needs.
The 5 Rs
- Right patient: Is this the correct patient for this medication?
- Right medication: Is this the appropriate medication for the patient’s condition?
- Right dose: Is this the correct dose for the patient?
- Right time: Is this the appropriate time to administer the medication?
- Right route: Is this the correct route for administering the medication (eg. oral, intravenous)?
Dispensing and preparation: good practice
Reporting patterns also highlight errors during the dispensing and preparation stages as areas of concern. Asking the right questions and following established procedures helps ensure that medications are prepared and dispensed safely. Key questions include:
- Labelling: Is the medicine correctly labelled with the patient’s name, date of birth, and dosage instructions?
- Storage: Are there any special storage requirements for the medicine (eg. refrigeration)
- Dosage: Is the dosage appropriate for the patient?
- Interactions: Could this medicine interact with other medications, herbal medicines, natural remedies, supplements, or certain foods?
- Instructions: Are there clear guidelines for the patient on how to take the medicine?
Encouraging reporting of medication errors
Reporting medication errors should be about learning and prevention, not assigning blame. Creating a safe reporting culture, protecting anonymity, and recognising those who actively report can all help improve medication safety. While medication errors are often reported to patient safety organisations, pharmacovigilance centres can fill this gap where no such system exists. To encourage reporting:
✓ Protect anonymity where possible to encourage open reporting.
✓ Recognise and reward those that actively report and improve medication safety.
✓ Make it easy for patients, carers, and healthcare professionals to report medication errors.
Problematic medication groups
Monitoring how medicines are used is key to preventing medication errors. Double-checking dosages and patient instructions can greatly reduce the risk of errors. Here are some of the most well-known groups of medications where errors can have serious consequences:
- Blood thinners: Anticoagulants help prevent heart attacks, strokes, and blood clots. But they can also increase the risk of serious bleeding.
- Insulin and other diabetes medications: These medications help manage blood sugar levels. However, incorrect dosing can cause complications such as hypoglycaemia (low blood sugar).
- Non-steroidal anti-inflammatory drugs (NSAIDs): Commonly used to relieve pain and inflammation, NSAIDs can cause gastrointestinal bleeding and kidney problems, especially when taken in high doses or for long periods.




Beyond medicines: Expanding the definition of medication errors
Medication errors aren’t limited to medicines. They can occur in these areas as well:
- Vaccines: Errors in the storage, handling, or administration of vaccines.
- Medical devices: Errors related to the use of devices such as infusion pumps, insulin pens, or inhalers.
- Supplements: Issues arising from the use of dietary supplements, including interactions with prescribed medications.
- Diagnostics: Errors in diagnostic processes, such as misinterpreting test results, can lead to incorrect treatment plans.
Read more
Making fewer medication errors – Education and training remain key, Uppsala Reports.
Medication error reporting for patients in Africa – the time to act is now, Uppsala Reports.
Mind the gap: Preventing medication errors after hospital discharge, Uppsala Reports.
International Medication Safety Network (IMSN) – Targeting medication errors, Uppsala Reports.

